Healthcare organizations face constant threats like ransomware, phishing, and insider risks, making cybersecurity a necessity to protect sensitive patient data. Compliance with regulations like [HIPAA](https://en.wikipedia.org/wiki/Health_Insurance_Portability_and_ Accountability_Act) and HITRUST is non-negotiable, and failing to secure systems can result in fines, operational disruptions, and loss of patient trust. Below are eight actionable steps to strengthen cybersecurity:
- Conduct Regular Risk Assessments: Identify vulnerabilities in systems, devices, and third-party vendors.
- Implement Role-Based Access Controls (RBAC): Limit data access based on job roles to minimize exposure.
- Encrypt Patient Data: Protect data both during transmission and when stored.
- Use Multi-Factor Authentication (MFA): Add extra security layers to prevent unauthorized access.
- Train Employees on Security Awareness: Educate staff to recognize phishing and other threats.
- Monitor Networks for Threats: Use tools to detect and respond to suspicious activity in real time.
- Manage Third-Party Risks: Evaluate and monitor vendors to ensure their security practices align with your standards.
- Create Backup and Disaster Recovery Plans: Ensure data can be restored quickly during a cyberattack or system failure.
These measures provide a solid framework for safeguarding patient information and maintaining operational continuity. Regular updates and training are key to staying ahead of evolving threats.
1. Conduct Regular Risk Assessments
Regular risk assessments are essential for identifying new threats and vulnerabilities. This step lays the groundwork for a solid cybersecurity strategy. For healthcare organizations, it means figuring out where patient data resides, who can access it, and what potential risks exist.
Begin by pinpointing every location where protected health information (PHI) is stored - whether it's electronic health records, billing systems, patient portals, or backup servers. Then, map how data flows between departments, vendors, and cloud services. Without a clear picture of where your data lives, it’s impossible to protect it effectively.
Evaluate the likelihood and potential impact of threats like ransomware, phishing attacks, or unsecured devices. Use this analysis to decide where to focus your resources.
Document any vulnerabilities, the controls you have in place, and any gaps that remain. This documentation is not just for internal use - it’s critical for audits and proving that your organization is taking cybersecurity seriously.
Compliance with [HIPAA](https://en.wikipedia.org/wiki/Health_Insurance_Portability_and_ Accountability_Act) and HITRUST
Healthcare organizations are required to conduct regular risk assessments under HIPAA, which demands that risks and vulnerabilities be identified and mitigated. HITRUST goes a step further by mandating a structured risk assessment methodology that aligns with multiple regulatory standards. The HITRUST Common Security Framework (CSF) ensures that organizations address administrative, physical, and technical safeguards comprehensively.
These assessments also create a paper trail for audits. The Office for Civil Rights (OCR) looks for evidence of ongoing risk management during HIPAA audits. Missing or outdated assessments can lead to penalties and enforcement actions.
Tackling Healthcare-Specific Threats
Healthcare systems face unique challenges. Many medical devices - such as infusion pumps, imaging machines, and patient monitors - are connected to networks but often run on outdated software that can’t be easily updated. A thorough risk assessment helps identify these weak points.
Insider threats are another concern. Employees with legitimate access to patient data might misuse it, whether intentionally or accidentally. Risk assessments should review access patterns, privilege levels, and monitoring systems to detect unusual behavior before it escalates.
Third-party vendors also bring risks. Whether it’s billing companies, cloud storage providers, or medical transcription services, any external partner handling PHI needs to be evaluated. Assessments should extend beyond your organization to include vendor security practices and contractual safeguards.
Simple Implementation for Healthcare Providers
Risk assessments don’t require complex tools to get started. Small clinics can use basic questionnaires and checklists to uncover common security gaps. The Department of Health and Human Services even provides free tools tailored for smaller providers.
Larger healthcare systems can benefit from automated scanning tools that continuously monitor for vulnerabilities. These tools integrate with existing IT systems, offering real-time insights without disrupting daily operations.
The key is to make risk assessments a regular part of your workflow. Schedule them quarterly or whenever major changes occur, like new software installations, facility expansions, or changes in business partnerships.
Scaling for Organizations of All Sizes
The approach to risk assessments can vary depending on the size of the organization:
- Small practices can focus on simple measures like strong passwords, antivirus software, securing physical devices, and basic employee training. These assessments might only take a few hours using straightforward templates.
- Mid-sized organizations often need a more structured approach, involving collaboration between IT teams, compliance officers, and clinical leadership. Assessments should cover technical controls, policies, and operational processes.
- Large health systems require enterprise-level frameworks to coordinate risk assessments across multiple facilities and departments. These organizations usually have dedicated risk management teams and use advanced platforms to track vulnerabilities, remediation efforts, and compliance.
Regardless of size, the goal remains the same: understand your risks, prioritize the most pressing issues, and take action to safeguard patient data. When done regularly, risk assessments transform cybersecurity from an abstract concern into a manageable and measurable process.
With risks clearly identified, healthcare organizations can move on to implementing stronger access controls for securing sensitive data.
2. Use Role-Based Access Controls (RBAC)
After conducting thorough risk assessments, implementing Role-Based Access Controls (RBAC) is a key step in safeguarding sensitive healthcare data. RBAC works by restricting access to patient information based on an employee’s job responsibilities. For instance, a nurse typically doesn’t need access to billing details, and a receptionist wouldn’t require access to clinical notes. This approach ensures that staff members only interact with the data they need to perform their roles effectively. By limiting access, RBAC reduces the risk of unauthorized data exposure and curtails the impact of compromised credentials or insider threats.
To put RBAC into practice, start by defining roles - such as physicians, nurses, administrative staff, billing specialists, IT administrators, and contractors - and clearly document the permissions associated with each. Assign employees to these predefined roles to streamline access management and minimize errors.
Compliance with HIPAA and HITRUST
RBAC also plays a crucial role in meeting compliance standards like HIPAA and HITRUST. HIPAA’s Security Rule mandates that healthcare entities implement strict access controls to protect electronic protected health information (ePHI). This includes requirements for unique user IDs, emergency access protocols, and automatic logoff features. HITRUST further emphasizes the importance of maintaining documented access rights, conducting regular reviews, quickly revoking access when roles change, and maintaining detailed audit logs to detect suspicious activity.
Addressing Healthcare-Specific Threats
Healthcare organizations are prime targets for both external attacks and internal misuse. RBAC can significantly reduce risks in these scenarios. For example, if a phishing attack compromises a receptionist’s login credentials, RBAC ensures that the attacker cannot access sensitive clinical records. Additionally, monitoring tools can flag any attempts to access information outside the user’s assigned role, further reducing threats like medical identity theft.
Implementing RBAC in Healthcare Environments
Modern electronic health record (EHR) systems come equipped with built-in RBAC features, making implementation more manageable. These systems allow administrators to create custom roles with precise permissions. To ensure proper setup, start with a role inventory, consult department heads, and test configurations with a small group before rolling out the system organization-wide. Avoid simply copying legacy permissions, as these often grant excessive access. Regular audits - ideally conducted quarterly - are essential to address changes in roles and prevent vulnerabilities from outdated or orphaned accounts.
Adapting RBAC for Different-Sized Organizations
RBAC can be tailored to fit healthcare organizations of all sizes. Smaller clinics can implement RBAC with just a few roles, such as physician, nurse, administrative staff, and IT support, providing a significant security boost compared to unrestricted access. Mid-sized organizations may need more detailed role hierarchies, accommodating departments like cardiology, pediatrics, or radiology. For larger health systems, RBAC should integrate into a broader enterprise cybersecurity strategy capable of handling the complexities of IoT devices and expanding connectivity. Regardless of the organization’s size, the core principle remains the same: align data access with job functions, document permissions thoroughly, and regularly review access rights to maintain both security and operational efficiency.
Once RBAC is in place, take the next step in securing patient data by implementing strong encryption protocols.
3. Encrypt Patient Data in Transit and at Rest
Encryption transforms sensitive patient information into unreadable data, accessible only with the correct decryption key. This protection is essential for two key scenarios: data in transit (when it’s being transmitted between systems, devices, or networks) and data at rest (when stored on servers, databases, or backup systems). Without encryption, patient records are at risk of interception during transfer or theft from storage systems.
A study conducted for 2024–2025 revealed that all compromised health data was unencrypted, highlighting just how critical encryption is for safeguarding sensitive information. It acts as a vital layer within a broader security framework.
Compliance with HIPAA and HITRUST
Under HIPAA, encryption is classified as an "addressable" measure for securing transmitted and stored data. This means organizations must either implement encryption or provide documented justification for an alternative approach. However, with the growing sophistication of cyber threats and the availability of effective encryption tools, opting out is increasingly difficult to justify.
HITRUST integrates encryption into its Common Security Framework (CSF), requiring organizations to encrypt electronic protected health information (ePHI) using industry-standard algorithms for both storage and transmission. Regular audits ensure encryption keys are securely managed and that decryption access is tightly controlled.
How Encryption Mitigates Healthcare-Specific Risks
Encryption is a powerful defense against many healthcare-related threats. For example, if unauthorized individuals gain physical access to servers, laptops, or mobile devices containing patient data, encryption ensures the information remains unreadable without the appropriate decryption key. When paired with role-based access controls (RBAC), encryption adds another layer of protection, ensuring that even if unauthorized access occurs, the data remains secure.
It also significantly reduces the risk of medical identity theft. Even if other security measures are compromised, encrypted data is essentially useless without the means to decrypt it. This protection works hand in hand with RBAC and network segmentation, creating a robust, multi-layered defense.
Simplified Implementation in Healthcare Settings
Advances in healthcare technology have made encryption easier to implement than ever before. Many electronic health record (EHR) systems now come with built-in encryption for data at rest, often enabled by default or requiring minimal setup. For data in transit, secure protocols like Transport Layer Security (TLS) are now standard for web-based and system-to-system communications.
To fully secure patient data, healthcare providers must first identify all locations where information is stored, including servers, workstations, mobile devices, cloud systems, and backups. Enable full-disk encryption on these endpoints and ensure EHR systems are configured to encrypt database files. For cloud storage, confirm that the provider offers encryption at rest in compliance with HIPAA standards.
For data in transit, use TLS 1.2 or higher, and disable outdated protocols. Email and file transfers should always utilize encrypted channels, such as SFTP, rather than unsecured alternatives.
Proper management of encryption keys is critical. Establish clear procedures for key generation, storage, rotation, and revocation. Tools like hardware security modules (HSMs) or cloud-based key management services can simplify this process while ensuring compliance.
Scalable Solutions for Organizations of All Sizes
The Healthcare Cybersecurity Act of 2025 requires encryption solutions to be scalable, with CISA offering resources tailored to healthcare practices of varying sizes.
- Small clinics and independent practices can often implement encryption without major investments, as many cloud-based EHR systems include encryption by default. Managed service providers can assist with setup and maintenance, focusing on protecting critical assets like patient databases, backups, and portable devices.
- Mid-sized organizations benefit from integrating encryption into their existing security frameworks. Many enterprise security platforms now offer unified encryption management alongside other tools, streamlining operations and boosting efficiency.
- Large health systems face the challenge of securing data across multiple facilities and interconnected systems. Secure cloud solutions provide scalable and flexible encryption options, making them ideal for enterprise-level deployments. For legacy medical devices that can’t support modern encryption, network segmentation can isolate these systems, ensuring data is protected once it enters compliant infrastructures.
No matter the size of the organization, encryption should always be paired with strict access controls. Identity and Access Management (IAM) systems ensure that even if encrypted data is accessed, proper authentication and authorization are required to decrypt it. Combining encryption with access controls, network segmentation, and monitoring creates a defense strategy that adapts to an organization’s unique needs.
To further secure access to systems, implementing multi-factor authentication is a must.
4. Deploy Multi-Factor Authentication (MFA)
Once data is protected with encryption, the next crucial step is strengthening user authentication by implementing Multi-Factor Authentication (MFA). MFA adds an extra layer of security by requiring multiple forms of verification, such as a fingerprint, a unique code sent to a device, or a hardware token.
This added layer is especially effective at reducing the risk of stolen credentials - one of the most common attack methods in healthcare - even when sensitive data is encrypted.
MFA also plays a vital role in Identity and Access Management (IAM) systems. For example, healthcare payers have successfully used MFA within their IAM frameworks to secure processes like user registration, access to claims, and credential management. Incorporating MFA into your IAM strategy lays a strong foundation for security and is a necessary step before advancing to more comprehensive measures, such as staff training programs.
5. Train Employees on Security Awareness
While technical defenses like multi-factor authentication (MFA) offer solid protection, employees often represent a weak link in healthcare cybersecurity. Actions like clicking on phishing emails, opening malicious attachments, or falling victim to social engineering can unintentionally expose sensitive systems and patient data to cybercriminals. Regular security awareness training addresses this issue by empowering healthcare workers with the skills to detect and prevent cyberattacks before they lead to data breaches.
Tackling Healthcare-Specific Threats
Security awareness training directly addresses the threats healthcare staff face daily. These programs teach employees how to spot phishing attempts, such as emails with suspicious attachments or links from unknown senders. Staff are trained to verify unusual email requests through trusted channels and to report anything suspicious immediately. By equipping employees with this knowledge, organizations can significantly reduce the chances of malware or ransomware infiltrating their systems.
Simple Integration into Healthcare Workflows
Effective security training doesn’t have to be complicated. Start by offering regular, straightforward sessions that cover key topics like identifying threats, handling sensitive information responsibly, and reporting potential issues. These sessions should be scheduled consistently throughout the year and updated to address new risks as the cybersecurity landscape evolves.
To create a culture of cybersecurity, healthcare organizations should encourage open communication and ensure employees feel comfortable reporting concerns without fear of repercussions. When staff understand their role in safeguarding patient information, the organization as a whole becomes better equipped to handle cyber threats.
As employees grow more confident in recognizing risks, healthcare providers can complement this knowledge with advanced technical defenses.
Meeting HIPAA and HITRUST Requirements
Security awareness training isn’t just a good idea - it’s required under HIPAA. The HIPAA Security Rule mandates that all workforce members, including management, participate in security awareness and training programs. Regular training demonstrates an organization’s dedication to compliance and ensures employees understand their responsibilities when handling protected health information (PHI). Key topics include proper management of electronic PHI, password security, and the consequences of security violations.
For organizations aiming for HITRUST certification, documented training programs are essential. Detailed records, including attendance logs and assessment results, provide auditors with clear evidence of ongoing efforts to improve security practices.
sbb-itb-ec1727d
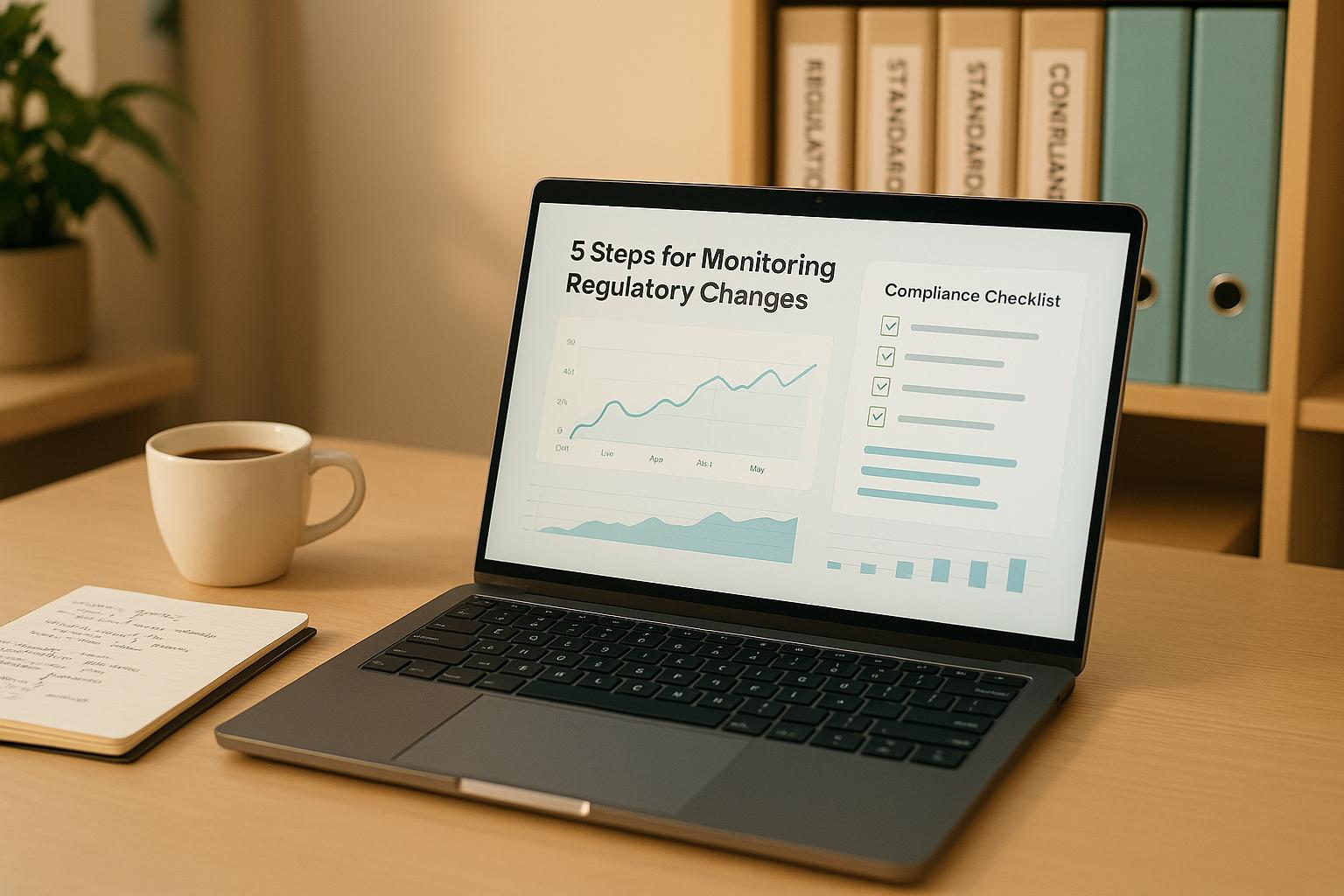
6. Monitor Networks and Detect Threats
Keeping a close eye on your network is crucial for catching threats early. Even with encryption and RBAC (Role-Based Access Control) in place, some risks can slip through the cracks. That's where network monitoring and threat detection tools come in. They provide real-time insights into suspicious activity, enabling IT teams to act quickly and stop small issues from turning into major security incidents.
Tackling Healthcare-Specific Cyber Threats
Healthcare organizations face a unique set of cybersecurity challenges. From medical devices connected to hospital networks to electronic health record (EHR) systems managing thousands of patient files, the environment is highly complex. Add in multiple access points across various departments, and it's clear why continuous monitoring is a must. It helps spot unusual behavior, like unauthorized access attempts, unexpected data transfers, or logins from unfamiliar locations.
Modern threat detection tools take this a step further by using behavioral analysis to identify anomalies that traditional tools might overlook. For example, if a user account suddenly accesses a large number of patient records outside regular working hours or if data starts transferring to an external server without approval, these tools flag the activity for immediate investigation. This proactive approach helps stop ransomware attacks and prevents sensitive data from being stolen.
Network segmentation adds another layer of protection by isolating systems and limiting how far an attacker can move within the network. For instance, if a workstation in the billing department is compromised, monitoring tools can alert the security team if that device tries to access the EHR database or other restricted areas. Together with encryption and RBAC, these monitoring practices create a strong, unified defense.
Implementing Monitoring in Healthcare Settings
The good news? You don’t need to overhaul your entire system to implement network monitoring. Security Information and Event Management (SIEM) tools make it easier by collecting logs from firewalls, servers, and endpoints, and presenting everything in a centralized dashboard for real-time analysis.
Start by focusing on critical assets like EHR systems, patient databases, and medical imaging devices. Install monitoring agents or configure existing devices to send logs to your SIEM platform. Many healthcare organizations begin with their most sensitive systems and expand monitoring as they gain experience and resources.
Automated alert systems also play a key role by reducing false alarms and ensuring that genuine threats get immediate attention. You can customize alerts to match healthcare-specific scenarios, like repeated failed login attempts, terminated employees trying to access patient records, or connections from known malicious IPs. This targeted approach avoids overwhelming your team with unnecessary alerts while keeping critical threats front and center.
Integration with existing security tools strengthens your defenses further. For instance, if monitoring tools detect suspicious activity, they can automatically isolate affected devices, block harmful IPs, or require extra authentication for accessing sensitive data. This automation cuts down the time between detecting and containing threats.
Staying Compliant with HIPAA and HITRUST
Healthcare organizations must comply with strict regulations like HIPAA, which requires detailed logging of system activities. Logs need to be retained for at least six years and reviewed regularly to spot unauthorized access or other violations involving Protected Health Information (PHI).
Network monitoring tools make this process easier by generating the comprehensive audit trails needed for compliance. These logs record who accessed what, when they accessed it, and what actions they performed. During audits, you can demonstrate compliance by showing detailed records of system activity and evidence of regular log reviews.
For organizations pursuing HITRUST certification, the requirements are even stricter. HITRUST demands continuous monitoring, real-time responses to security events, and thorough documentation. Automated monitoring systems help meet these standards by maintaining detailed records without relying solely on manual processes. Regular log reviews also help identify policy violations, such as employees accessing patient records without a valid reason, allowing organizations to address these issues proactively.
Scalable Solutions for All Healthcare Organizations
Network monitoring solutions are flexible enough to meet the needs of healthcare providers of all sizes. Small clinics with limited IT resources can start with cloud-based services that handle log collection and analysis behind the scenes. These platforms are user-friendly, even for non-technical staff.
Mid-sized organizations often benefit from a hybrid approach, combining cloud-based monitoring for scalability with on-premises tools for sensitive systems. This setup ensures direct control over critical data while still taking advantage of advanced cloud features. Adding new devices or locations is usually a straightforward process as the organization grows.
Large hospital networks require enterprise-grade solutions capable of handling vast amounts of data from thousands of devices. These systems often include machine learning to refine threat detection by understanding normal network behavior. Many large organizations also operate Security Operations Centers (SOCs) staffed with analysts who monitor alerts 24/7.
To ensure your monitoring system is working as intended, conduct regular tests. Review alert configurations, verify that logs are being collected from all critical systems, and simulate security incidents to confirm the tools are detecting and reporting threats properly. These routine checks ensure your network monitoring remains effective and supports your broader security strategy.
7. Manage Third-Party and Vendor Risk
Healthcare organizations depend on a web of vendors, business associates, and third-party providers to handle everything from patient care to billing systems, data storage, and medical device maintenance. While these partnerships are essential, they bring along a major challenge: security risks. A single weak link in this network can compromise thousands of patient records, potentially jeopardizing the entire operation.
In fact, over 80% of stolen PHI (Protected Health Information) records are linked to breaches involving third-party vendors, software services, business associates, and non-hospital providers. A stark example is the 2024 UnitedHealth Group/Change Healthcare ransomware attack, which led to the theft of 192.7 million Americans' healthcare records. These breaches weren’t caused by hospitals neglecting their own systems but by attackers exploiting vulnerabilities within the vendor ecosystem. These incidents highlight the pressing need for a solid vendor risk management strategy.
Tackling Healthcare-Specific Threats
Each third-party connection adds another layer of vulnerability, increasing the surface area for potential cyberattacks. Because healthcare systems are so interconnected, a breach in one vendor’s system can ripple across the entire network, disrupting operations, draining finances, and even endangering patient safety.
One of the biggest hurdles healthcare organizations face is the lack of visibility into their data landscape - where it’s stored, who has access, and how much is being held. Without this clarity, securing sensitive data becomes nearly impossible. Many organizations only realize a vendor has been storing critical patient information on unsecured servers after a breach occurs.
The financial toll is sobering. In 2024, the average cost of a data breach in healthcare reached $9.77 million per incident, making it the most expensive sector for breaches since 2011. These costs include regulatory fines, legal battles, patient notifications, credit monitoring, and operational disruptions.
To address these risks, start by building a comprehensive third-party risk management program. Identify every vendor that interacts with patient data - cloud storage providers, billing services, medical device manufacturers, telehealth platforms, and even contractors with remote access. Once you know who’s in your ecosystem, evaluate their security practices. Request documentation on their security measures, incident response plans, and compliance certifications. For technology vendors, insist on a Software Bill of Materials (SBOM) to understand what’s inside their software, including third-party components that could pose risks.
Aligning with HIPAA and HITRUST
HIPAA requires business associates to protect PHI, meaning your organization is legally accountable for vendor-related breaches. If a vendor suffers a breach, your organization could face regulatory investigations and penalties.
Business Associate Agreements (BAAs) are a critical safeguard. These contracts should clearly outline security responsibilities, breach notification protocols, and audit rights. However, signing a BAA isn’t enough - you must ensure vendors are actually meeting their obligations. Regular audits are essential to verify compliance with agreed-upon security standards. Like encryption and role-based access controls (RBAC), ongoing vendor oversight is a key part of any cybersecurity strategy.
For organizations pursuing HITRUST certification, vendor management is even more demanding. The 2025 Healthcare Cybersecurity Benchmarking Study revealed that "Vendor/Supplier Cybersecurity Requirements" are often underdeveloped among the HPH Cybersecurity Performance Goals (CPGs). This gap poses a compliance risk, especially as third-party breaches continue to rise.
Maintaining an updated inventory of your data, networks, applications, and devices is crucial. This includes tracking network-connected medical devices and data held by third-party providers. By consistently mapping data flows, you can spot unauthorized access or usage by vendors before it becomes a problem.
Practical Implementation in Healthcare Settings
Introducing vendor risk management doesn’t mean overhauling everything. Start with your riskiest vendors - those with direct access to patient databases, EHR systems, or critical infrastructure. Focus on vendors handling large amounts of PHI or providing services essential to patient care.
Develop a standardized questionnaire to evaluate key security measures like encryption, access controls, and incident response. Use this tool for both new and existing vendor relationships, conducting annual reviews for high-risk vendors and less frequent reviews for lower-risk ones.
Automated vendor risk management platforms can simplify this process. These tools centralize vendor documentation, track assessment schedules, and flag vendors that fall short of security requirements. They also integrate with your existing compliance processes, reducing the manual effort involved in managing numerous vendor relationships.
Scaling for Organizations of All Sizes
Whether you’re a small clinic or a sprawling hospital network, your vendor risk strategy needs to be tailored to your size. Small clinics might focus on their top three to five vendors, while mid-sized organizations can categorize vendors by risk for periodic reviews. Larger systems often need dedicated teams and real-time monitoring tools.
Big hospital networks typically have formal vendor risk management programs with specialized staff and advanced tools. These organizations may require vendors to hold specific security certifications, undergo regular penetration testing, and provide real-time security updates. Some large systems are even consolidating their cybersecurity tools onto unified platforms for greater efficiency, though this approach needs careful oversight to avoid creating new vulnerabilities.
8. Create Backup and Disaster Recovery Plans
When ransomware or other disasters strike, the ability to restore patient data and maintain care is critical. Without dependable backups, healthcare services can grind to a halt, disrupting patient care and putting lives at risk.
A solid backup and disaster recovery plan ensures that patient care continues even during system failures. This involves keeping multiple copies of essential data, routinely testing those backups, and having clear steps in place to restore operations quickly.
In healthcare, downtime has real-world consequences. Emergency departments need instant access to allergy information, medication histories, and treatment plans. Surgeons rely on imaging systems and electronic health records during procedures. If these systems fail, patient safety is immediately at stake.
Addressing Healthcare-Specific Threats
Ransomware attacks are a major reason healthcare organizations invest in robust backup strategies. Cybercriminals target hospitals because they know patient care is on the line, often leading organizations to pay hefty ransoms. A strong backup plan removes this leverage - if you can restore systems from clean backups, you can avoid paying.
The 3-2-1 backup rule is a practical approach:
- Keep three copies of your data,
- Use two different types of storage media, and
- Store one copy offsite.
For healthcare, this might mean keeping production data on primary servers, creating nightly backups to network-attached storage, and storing encrypted copies in a secure cloud or remote data center.
But having backups isn't enough. Modern ransomware can target backups, encrypting or destroying them. To counter this, healthcare organizations need immutable backups - unchangeable copies that can't be altered or deleted. These "write-once, read-many" backups remain safe even if attackers gain access to your systems.
Additionally, backups that aren't tested are unreliable. Quarterly testing under realistic conditions is essential to identify gaps. These tests should measure how long it takes to restore systems and ensure all critical data is covered. Define clear recovery goals, such as a Recovery Time Objective (RTO) of two hours for electronic health records and a Recovery Point Objective (RPO) of 15 minutes for critical systems.
Meeting HIPAA and HITRUST Standards
HIPAA's Security Rule mandates that healthcare organizations have procedures for creating and maintaining exact copies of electronic protected health information (ePHI). This includes having documented processes for restoring data during an incident, making backup plans a compliance necessity.
If a third party manages your data, your Business Associate Agreement (BAA) must outline backup responsibilities. For example, if a cloud provider stores patient records, the BAA should specify how often backups occur, how long they are retained, and how restoration will be handled. Even when outsourcing, your organization remains responsible for HIPAA compliance, so it's crucial to verify your vendor's practices.
HITRUST certification goes further, requiring documented backup processes, regular testing, and proof that backups can successfully restore operations. It also demands that backup data is encrypted and secured just like production data. Organizations must show that backups are integrated into their overall security measures.
Retention policies add complexity. While HIPAA doesn't specify exact retention periods, many states require medical records to be kept for six to ten years. Your backup strategy must account for this, ensuring long-term storage while keeping older backups accessible as technology evolves. This may involve migrating data to updated formats and maintaining detailed documentation on backup and restoration processes.
Practical Implementation in Healthcare
Start by identifying your most critical systems, such as electronic health records (EHR), practice management software, and systems that directly support patient care. Ensure these have reliable, tested backups before addressing less critical infrastructure.
Cloud-based backup solutions simplify implementation. These services handle scheduling, encryption, and offsite storage automatically, reducing the need for dedicated backup infrastructure. Many healthcare-focused platforms even integrate directly with popular EHR systems, streamlining the backup process.
Document your backup procedures thoroughly, including details like backup locations, encryption keys, and vendor contact information. Keep these instructions secure but accessible - ideally in multiple formats, including printed copies, since network access may be unavailable during a disaster.
Automated backups are a must. Manual backups depend on staff remembering to initiate them, which can fail during busy periods or staff changes. Automated systems run on schedules, send alerts for failures, and maintain logs of successful backups. Configure notifications to reach multiple team members to ensure issues are promptly addressed.
Scaling for Organizations of All Sizes
Smaller clinics with limited IT resources can start with straightforward setups, such as local network-attached storage for daily backups combined with a cloud service for offsite copies. The key is consistency - schedule regular backups and test restorations quarterly. Even a single-physician practice should aim to restore patient records within 24 hours of a failure.
Mid-sized organizations, like multi-location practices or small hospitals, often need more advanced solutions. These might include backup servers at each location with automated replication to a central data center. Centralized backup management tools can help monitor and verify backups across multiple sites.
Large hospital systems require enterprise-level disaster recovery plans. This often involves redundant data centers with real-time data replication, enabling failover within minutes. Continuous data protection systems can capture every change to critical applications, reducing recovery point objectives to near-zero.
Geographic distribution is crucial for larger organizations. Storing backups in different regions protects against localized disasters like hurricanes or wildfires. Some health systems even form reciprocal agreements with others, allowing operations to resume at partner facilities if primary locations are compromised.
Annual disaster recovery exercises are essential for all healthcare organizations. These simulations test your team's ability to execute recovery plans under pressure, whether facing a ransomware attack, natural disaster, or hardware failure. Use the lessons from these exercises to refine your procedures and strengthen your resilience over time.
Conclusion
Protecting patient data and maintaining operational continuity in healthcare demands a multi-layered approach to cybersecurity.
Risk assessments help identify weak points, while role-based access controls limit who can access sensitive data, reducing risks from insider threats or stolen credentials. Encryption ensures that even if data is stolen, it can’t be used, and multi-factor authentication (MFA) adds a crucial barrier against unauthorized access. Staff training to recognize threats and consistent network monitoring provide proactive defenses against breaches. Additionally, managing vendor risks and having solid backup plans ensure that patient care continues uninterrupted, even during cyber incidents. Together, these measures form a strong security framework that supports the technical safeguards discussed earlier.
These strategies also align closely with HIPAA and HITRUST compliance requirements. Compliance frameworks emphasize risk assessments, access controls, encryption, and backups because they provide proven security benefits. However, treating compliance as merely a checklist rather than a genuine effort to improve security leaves organizations exposed to threats.
It’s important to remember that technology alone isn’t enough to address cybersecurity challenges. Even the most advanced monitoring systems are ineffective if no one acts on alerts. Encryption won’t protect data if employees share passwords or fall for phishing scams. The key is combining the right tools with clear policies, ongoing training, and fostering a culture where everyone understands their role in protecting security. These layers of defense complement the best practices outlined earlier.
Healthcare organizations should prioritize based on their specific needs. For smaller clinics, starting with employee training, MFA, and reliable backups can provide essential protection without requiring significant investments. Larger hospital systems, on the other hand, may need more extensive measures, including dedicated security teams and enterprise-level tools.
Cybersecurity isn’t static - new challenges emerge regularly. Regularly reviewing and updating defenses is critical to staying ahead. Schedule quarterly reviews to assess whether existing controls remain effective, identify new threats, and determine if additional training or resources are needed to maintain resilience. This ongoing effort ensures that healthcare organizations are prepared for whatever comes next.
FAQs
What are some cost-effective ways small healthcare practices can strengthen their cybersecurity?
Small healthcare practices can boost their cybersecurity without spending a fortune by focusing on straightforward, effective steps. One important measure is setting up multi-factor authentication (MFA), which adds an extra layer of security to sensitive systems. Another key step is regularly training employees to spot phishing scams and encouraging them to report any suspicious emails. Since human error is a major weak point, this training can make a big difference.
Other simple practices include enforcing strong password policies, ensuring software is consistently updated, and restricting access to sensitive information based on specific job roles. These practical actions can go a long way in reducing cybersecurity risks while keeping costs manageable.
What challenges do healthcare organizations face with third-party vendor risks, and how can they manage them effectively?
Healthcare organizations face a tough challenge when it comes to managing third-party vendor risks, especially as vendor-related breaches are becoming more common. These risks often arise from weak security measures, limited visibility into vendor systems, and the increasing complexity of interconnected technologies.
To tackle these issues, it's crucial for organizations to put a strong third-party risk management program in place. Key steps include:
- Keeping an up-to-date inventory of all third-party assets, such as hardware, software, and data storage systems.
- Conducting regular evaluations of vendors' security practices to ensure they align with industry standards like HIPAA.
- Drafting clear contracts that define cybersecurity expectations and responsibilities.
Taking a proactive approach to managing vendor risks helps healthcare organizations safeguard sensitive patient data and minimize vulnerabilities within their supply chain.
Why should healthcare organizations regularly update and test their backup and disaster recovery plans, and what are some best practices to follow?
Regular updates and routine testing of backup and disaster recovery plans are crucial for healthcare organizations. These measures ensure that critical systems and sensitive patient data can be restored swiftly in case of a cyberattack or system failure. By doing so, organizations can reduce downtime, maintain patient care, and stay compliant with regulations like HIPAA.
Some key practices include conducting frequent data backups, securing those backups in safe locations (such as encrypted, offsite storage), and running disaster recovery drills on a regular basis. Simulating realistic scenarios during these drills helps teams identify weaknesses and ensures they’re ready to respond effectively when it matters most.